
Bladder Prolapse
Introduction
Bladder prolapse, also known as cystocele, is a condition that many people are unaware of until it significantly impacts their daily lives. Understanding bladder prolapse is crucial for managing its symptoms and improving quality of life. Let’s delve into what bladder prolapse is, its causes, symptoms, and the various treatment options available.
Understanding Bladder Prolapse
What is Bladder Prolapse?
Bladder prolapse occurs when the bladder drops from its normal position and bulges into the vagina. This happens due to the weakening of the pelvic floor muscles and ligaments that support the bladder. It can range from mild to severe, depending on how far the bladder has descended.
How Common is Bladder Prolapse?
Bladder prolapse is relatively common, particularly among women who have given birth or are going through menopause. Studies suggest that up to 50{ca840de20a89c9df01ee67f664a5c1bef4377b6cdb5728d1ab774f0180b49f28} of women may experience some degree of pelvic organ prolapse in their lifetime, with bladder prolapse being one of the most common types.
Causes of Bladder Prolapse
Weakening of Pelvic Muscles
The primary cause of bladder prolapse is the weakening of the pelvic floor muscles and tissues. These muscles can lose strength due to several factors, leading to insufficient support for the bladder.
Childbirth
Childbirth is a significant risk factor for bladder prolapse. The process of labor and delivery can stretch and weaken the pelvic floor muscles, especially after multiple deliveries or deliveries involving large babies.
Menopause
Menopause contributes to bladder prolapse due to decreased estrogen levels, which can lead to the weakening of pelvic tissues and muscles.
Heavy Lifting and Chronic Coughing
Frequent heavy lifting and chronic coughing can increase abdominal pressure, straining the pelvic floor muscles and increasing the risk of bladder prolapse.
Symptoms of Bladder Prolapse
Physical Symptoms
Common physical symptoms include a feeling of fullness or pressure in the pelvis, a bulge in the vagina, and discomfort during physical activities or sexual intercourse.
Urinary Symptoms
Urinary symptoms can include difficulty starting urination, frequent urination, a sensation of incomplete emptying of the bladder, and urinary incontinence.
Sexual Symptoms
Bladder prolapse can cause discomfort or pain during sexual intercourse, affecting intimate relationships and overall sexual health.
Risk Factors for Bladder Prolapse
Age
The risk of bladder prolapse increases with age as pelvic floor muscles naturally weaken over time.
Family History
A family history of pelvic organ prolapse can increase the likelihood of developing bladder prolapse.
Obesity
Excessive body weight adds pressure on the pelvic floor muscles, raising the risk of prolapse.
Previous Pelvic Surgery
Surgeries such as hysterectomy can weaken pelvic floor support structures, leading to an increased risk of bladder prolapse.
Diagnosis of Bladder Prolapse
Physical Examination
A healthcare provider will perform a physical examination to assess the extent of the prolapse and check for other pelvic organ prolapses.
Pelvic Organ Prolapse Quantification System (POP-Q)
The POP-Q system is a standardized method used to quantify and describe the severity of pelvic organ prolapse.
Imaging Tests
Imaging tests like ultrasound, MRI, or cystourethrogram can help visualize the extent of bladder prolapse and identify any associated issues.
Stages of Bladder Prolapse
Stage 1: Mild
In mild cases, the bladder has dropped slightly but remains mostly within the vagina.
Stage 2: Moderate
Moderate prolapse involves the bladder descending to the opening of the vagina.
Stage 3: Severe
Severe prolapse is when the bladder bulges out of the vaginal opening.
Stage 4: Complete
Complete prolapse occurs when the bladder is completely outside the vaginal opening.
Complications of Bladder Prolapse
Urinary Tract Infections
Bladder prolapse can lead to frequent urinary tract infections due to incomplete emptying of the bladder.
Bladder Damage
Prolonged prolapse can cause damage to the bladder, affecting its function and health.
Impact on Quality of Life
The symptoms and complications of bladder prolapse can significantly impact a person’s quality of life, affecting physical comfort, emotional well-being, and social interactions.
Treatment Options for Bladder Prolapse
Non-Surgical Treatments
Pelvic Floor Exercises
Kegel exercises can strengthen the pelvic floor muscles and provide support to the bladder, helping to alleviate symptoms.
Pessaries
A pessary is a device inserted into the vagina to support the bladder and other pelvic organs, providing relief from prolapse symptoms.
Surgical Treatments
Anterior Vaginal Repair
This surgery involves tightening the pelvic floor muscles and tissues to lift the bladder back into place.
Vaginal Mesh Surgery
A mesh is used to support the pelvic organs and keep the bladder in its proper position. This procedure can be effective but has potential risks and complications.
Preventing Bladder Prolapse
Lifestyle Changes
Maintaining a healthy weight, avoiding heavy lifting, and managing chronic coughs can help reduce the risk of bladder prolapse.
Regular Exercise
Regular exercises, especially those targeting the pelvic floor, can strengthen the muscles and provide better support for the bladder.
Proper Lifting Techniques
Using proper lifting techniques, such as bending the knees and keeping the back straight, can prevent excessive strain on the pelvic floor muscles.
Living with Bladder Prolapse
Managing Symptoms
Managing symptoms involves regular pelvic floor exercises, using pessaries if recommended, and avoiding activities that exacerbate the condition.
Emotional and Psychological Support
Living with bladder prolapse can be emotionally challenging. Seeking support from mental health professionals and joining support groups can be beneficial.
Support Groups and Resources
Joining support groups and utilizing resources like educational materials and counseling services can provide valuable information and emotional support.
Diet and Bladder Prolapse
Foods to Avoid
Avoiding foods and beverages that irritate the bladder, such as caffeine, alcohol, and spicy foods, can help manage symptoms.
Foods to Include
Including fiber-rich foods in the diet can prevent constipation, reducing strain on the pelvic floor muscles.
Importance of Hydration
Staying well-hydrated helps maintain bladder health and prevents urinary tract infections.
Exercises for Bladder Prolapse
Kegel Exercises
Kegel exercises involve tightening and relaxing the pelvic floor muscles, helping to strengthen them and provide better bladder support.
Yoga and Pilates
Yoga and Pilates can improve overall core strength and flexibility, benefiting pelvic floor health.
Core Strengthening Exercises
Exercises that target the core muscles, such as planks and bridges, can help improve pelvic floor support.
Myths and Facts about Bladder Prolapse
Common Misconceptions
There are many myths about bladder prolapse, such as it being an inevitable part of aging or that surgery is the only treatment option.
Scientific Facts
Understanding the scientific facts about bladder prolapse can help dispel myths and encourage effective management and treatment.
Conclusion
Bladder prolapse is a common condition that can significantly impact quality of life. Understanding the causes, symptoms, and treatment options is essential for managing this condition effectively. If you experience any symptoms of bladder prolapse, it’s important to seek medical advice to explore the best treatment options for you.
FAQs
Can bladder prolapse heal on its own?
In some mild cases, bladder prolapse can improve with pelvic floor exercises and lifestyle changes, but medical evaluation is essential.
Is surgery the only option for bladder prolapse?
No, there are non-surgical options such as pelvic floor exercises and pessaries that can help manage symptoms.
How long does it take to recover from bladder prolapse surgery?
Recovery time varies, but most people can return to normal activities within 6 to 8 weeks after surgery.
Can men experience bladder prolapse?
Bladder prolapse is rare in men due to their different pelvic anatomy, but they can experience other forms of pelvic organ prolapse.
Are there any long-term effects of bladder prolapse?
If left untreated, bladder prolapse can lead to chronic urinary issues and impact overall quality of life. Seeking treatment can help manage these effects.
Bleeding After Menopause
You May Also Like

Healthy Foods: A Comprehensive Guide to Nourishing Your Body
August 5, 2023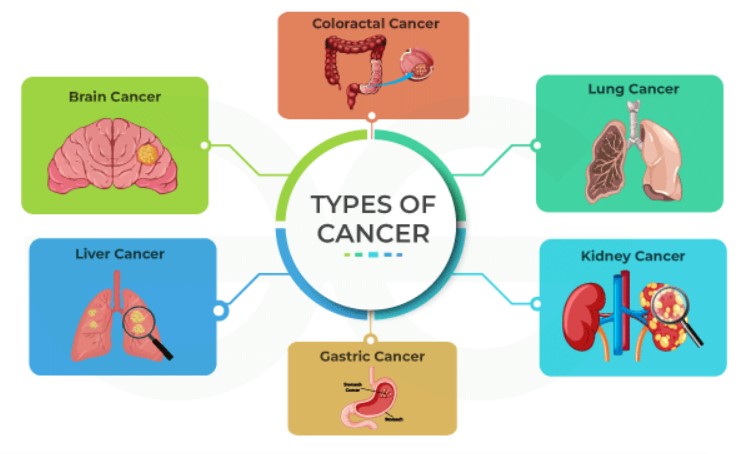
Understanding the Different Types of Cancer
November 12, 2023